Case Report - (2024) Volume 9, Issue 6
Background: Pyoderma Gangrenosum (PG) is a rare, neutrophilic, non-infectious, inflammatory dermatosis, clinically characterized by progressive necrotic and purulent tissue ulceration. In up to half of the cases the etiology remains idiopathic, whereas the other half of patients present with an underlying systemic disorder (inflammatory bowel disease, rheumatoid arthritis or lymphoproliferative disorder). The lower legs are most frequently affected although PG can present at any body site. Being a diagnosis of exclusion, there is often a failure of early detection. Innacurate diagnosis and treatment often cause the clinical overview to change, thus leading to progression.
Case presentation: A 49-year old, otherwise healthy, male patient presented with painful necrotic ulcers in lower extremities. He had been treated as pyodermia for two years. The edge-ulcer biopsy resulted in neutrophilic infliltrates. The patients condition showed great remission under systemic corticosteroids and immunosupressants.
Conclusion: This case highlights the challenges for early detection of pyoderma gangrenosum, considering the wide spectrum of differential diagnosis. Clinial determination of the morphological characteristics of the lesions, non-responding antibiotic treatment and improvement after corticosteroids should serve as guidance to early diagnosis and management of the disease.
Pyoderma gangrenosum • Non-healing wound • Ulceration • Corticosteroids
Pyoderma Gangrenosum (PG) is a rare, neutrophilic, non-infectious, inflammatory dermatosis, clinically characterized by progressive necrotic and purulent tissue ulceration. In up to half of the cases the etiology remains idiopathic, whereas the other half of patients present with an underlying systemic disorder (inflammatory bowel disease, rheumatoid arthritis or lymphoproliferative disorder). The lower extremities are the most predilection site of attack, however trunk, upper extremities and face may also be impacted. The diagnosis is based on the diagnostic criteria proposed by the international experts Delphi concensus, with the neutrophilic infiltrate findings on the biopsy, as the single major criterion to help establish the diagnosis [1].
We present a case of a 48 year old man who was referred to the dermatology clinic, after being unsuccessfully treated for months as pyodermia, with the complaints of ulcers in lower extremities accompained with pain. At first lesions had appeared on the chest and arms in the form of papules without any known trigger five years prior to the visit. Eversince the lesions had started to spread and cause pain, the patient had been using variety of unconventional medicine thus changing the appearance of the lesions. The patient was a chronic smoker. No other underlying condition has been detected [2].
On physical examination, lesions were located on the lower extremities, in the pretibial region presented as multiple, confluent and erythemo-ulcerative. The dimensions varied on the lateral site of the left leg 25 cm × 30 cm; on the posterior site 8 cm × 10 cm; on the lateral site of the right leg 18 cm × 10 cm. The latter were well demarked from the healthy skin. The ulcers’ base presented purulent, with pronounced granular tissue from the inside. The periphery was dominated by hemorragic crusts and necrotic tissue [3].
Laboratory tests, wound, throat and nose swabs for culture were taken, an abdomen ultrasound and colonocscopy were performed and a fragment of skin with dimensions 55 mm × 3 mm × 4 mm was taken for biopsy [4]. International experts Delphi concensus was used as a tool to evaluate the meeting of diagnostic criteria.
The edge-ulcer biopsy resulted in neutrophilic infliltrates, so the major single criterion was fullfilled. Additional six from the eight minor conditions to meet the criteria for Pyoderma gangrenosum were documented, including: Ruling out the presence of the infection, the presence of papules/ pustules/vesicules four days prior to the ulcer, peripheral erythema of the lesion, the presence of multiple ulcers, from which at least one in the anterior aspect of the calf and the reduction of the size of the lesion after the initiation of immunosupressant therapy. On addmision, sedimentation rate was 80 mm/Hg and the reactive C-protein was 56. Colonoscopy resulted within norms. Parenteral treatment with methylprednisolone 80 mg/daily was started in week 0 [5]. Azathioprine 100 mg/daily was added in week 3. Parenteral antibiotics were given due to Pseudomonas auregionosa isolates in the wound. Aditionally, anticoagulants, NSAID, osteoprotectors, vitamins and protein-pumpi-inhibitors were given as adjuvant therapy and to lessen the side-effect of the corticosteroids. Topically, the lesions were treated with antibiotics, corticosteroids (III class potency), epithelising cream and antiseptics. Debridement of the wound was done on the third week to remove the necrotic tissue. The removal of the necrotic tissue contributed in the precipitation of the ulcers thus stimulating epithelization. The treatment evaluation was done every two weeks after the initiation of the therapy. The progress of ulcerations was stopped. The patient achieved healing of all three ulcers in 13 weeks of therapy. The dosage of corticosteroids was gradually reduced to 30 mg/d and 50 mg/d of azhathioprine in the discharge day. The maintenance corticosteroid dose was 5 mg/daily. With the purpose of avoiding the corticosteroid long term side effects, treatment with dapsone, 100 mg/daily was initiated. In the 8 week follow up, the condition deteriorated. A return to systemic corticosteroids and immunosuppressants was necessary (Figures 1-5) [6].
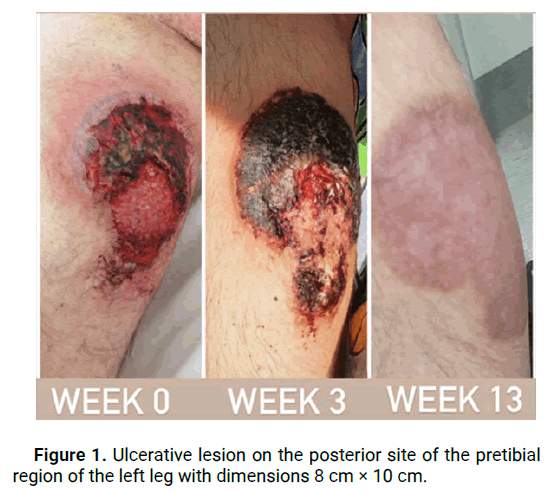
Figure 1: Ulcerative lesion on the posterior site of the pretibial region of the left leg with dimensions 8 cm × 10 cm.

Figure 2: Ulcerative lesion on the posterior site of the left leg in femoral region with dimensions 25 cm × 10 cm.

Figure 3: Ulcerative lesion on the lateral site of the right leg in the pretibial region with dimensions 18 cm × 10 cm.
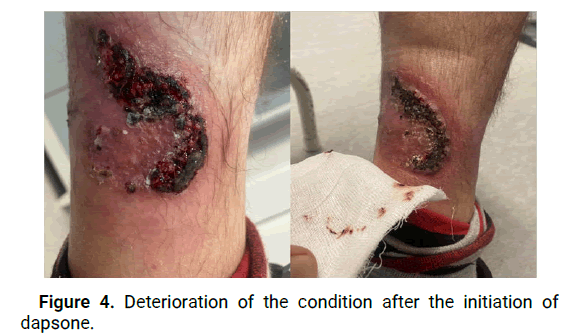
Figure 4: Deterioration of the condition after the initiation of dapsone.

Figure 5: Week 8 after interruption of dapsone and re-initiation with systemic corticosteroids and immunosupressants.
Pyoderma Gangrenosum (PG) is a rare and challenging inflammatory dermatosis that presents with progressive necrotic and purulent tissue ulceration [7]. The incidence and disease associations of PG wew investigated in the United Kingdom through a retrospective cohort study by Langan, et al. The study provided valuable epidemiological data, demostrating that PG in not only a rare condition but also associated with several underlying systemic disorders. This emphasizes the importance of considering PG as a potential complication in patients with these systemic conditions. Alavi, et al., discussed the importance of early and accurate diagnosis, as delayed or inaccurate diagnosis can lead to disease progression and complications. Aditionally, they provided insights into evolving treatment approaches, including immunosupressive agents and biologics, which play a significant role in the management of PG.
George, et al., emphasize the challenges in diagnosing PG due to its wide spectrum of differential diagnoses and highlight the value of histopathological examination in confirming the diagnosis. Maverakis, et al., aimed to standardize the diagnosis and reduce misdianosis rates by proposing criteria for ulcerative PG through a Delphi consensus of international experts. To establish a definitive diagnosis, in our research we have utilized the diagnostic criteria proposed by the international experts Delphi consensus [8]. The edge-ulcer biopsy revealed neutrophilis infiltrates, satisfying the major criterion and six out of eight minor criteria were also met, confirming the diagnosis of PG. This highlights the importance of histopathological examination in differntiating PG from other ulcerative conditions [9]. According to Brooklyn, et al., early initiation of immunosuppressant therapy an wound care are essential components in PG management to prevent disease progression and promote ulcer healing. In our case, the patient’s response to systemic corticosteroids and immunosuppresants was remarkable, leading to great remission of the lesions [10].
In conclusion, Pyoderma Gangrenosum (PG) remains a challenging and rare dermatosis, characterized by progressive necrotic and purulent tissue ulceration. Early detection and accurate diagnosis are vital for appropriate management, but it is often hindered by the wide spectrum of differential dignoses and the lact of sepficic diagnostic tests. This case study light on the difficuties in recognizing PG, as the patient was initially misdiagnosed and received ineffective treatment for months. The diagnostic criteria proposed by the international experts Delphi concensus play a crucial role in establishing the diagnosis of PG. However, further research is needed to develop more specific and reliable diagnostic tools. A multidisciplinary approach involving dermatologists, rheumatologist and wound care specialists is essential to effectively manage PG.
The authors declare that there are no competing interests.
Written informed consent was obtained from the patient for the publication of his data and images.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Pajaziti A and Bunjaku G . "Challenges in Early Detection and Management of Pyoderma Gangrenosum: Case Study". Dermatol Case Rep, 2023, 8(5), 1-3.
Received: 04-May-2024, Manuscript No. DMCR-23-26329; Editor assigned: 07-May-2024, Pre QC No. DMCR-23-26329 (PQ); Reviewed: 15-May-2024, QC No. DMCR-23-26329; Revised: 22-May-2024, Manuscript No. DMCR-23-26329 (R); Published: 18-Jul-2024
Copyright: © 2023 Pajaziti A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.