Original Article - (2024) Volume 9, Issue 6
Purpose: This study examines the incidence and management of post-operative haemorrhage following outpatient dermatosurgery, with a particular focus on the differences between unilateral and bilateral surgery. With the increasing popularity of outpatient dermatosurgery, which is characterised by shorter waiting times, less administrative burden, and a faster return of patients to their usual environment, this study discusses both the benefits and challenges of this development.
Methods: In a prospective observational study of 105 patients undergoing outpatient dermatosurgery, data were collected on demographic characteristics, type of surgery, duration, technique used, and anticoagulant therapy. Particular attention was paid to the follow-up and management of post-operative haemorrhage. The statistical analysis focused on the correlation between the type of surgery and the occurrence of post-operative bleeding.
Results: The results show that with adequate management, outpatient dermatological surgery can achieve comparable to better results than inpatient surgery. Postoperative haemorrhage was rare in our study population and most cases were successfully treated. The study emphasises the importance of effective bleeding management, particularly in patients on anticoagulation. The results suggest that outpatient dermatosurgical procedures are a safe and efficient alternative to inpatient surgery, provided that the necessary measures to minimize the risk of bleeding are carefully implemented.
Conclusion: The study contributes significantly to the understanding of the safety and effectiveness of outpatient dermatological surgery and provides valuable insights for clinical practice. It underpins the need for individualised risk assessment and management to fully exploit the benefits of outpatient surgery while maintaining a high level of patient safety.
Haemorrhage • Dermatosurgery • Risk assessment • Outpatient surgical care • Exploit
Outpatient surgical care in dermatological surgery has become considerably more important in recent years.
The advantages are obvious: Shorter waiting times, less administrative work and a quick return to the patient's familiar surroundings. Compared to an inpatient stay, patients benefit from reduced exposure to hospital infections and accelerated recovery in their familiar surroundings.
In addition, costs are often lower in an outpatient setting, which is an advantage for both patients and the healthcare system.
However, outpatient care also brings challenges. Pos-toperative haemorrhage is a particularly critical issue. In contrast to the inpatient setting, where immediate intervention and monitoring are guaranteed, it can be more difficult to react quickly to complications in the outpatient setting. It is therefore all the more important to take measures to minimize the risk of post-operative bleeding from the outset [1].
Dermatosurgery has established itself as an integral part of dermatological care in recent decades, with a significant trend towards outpatient surgery. This development has many advantages, both for patients and for the healthcare system.
Patients value outpatient surgical care for its convenience, reduced administrative burden and the opportunity to recover in their familiar surroundings. In addition, outpatient surgery can reduce the burden on hospitals, shorten waiting times and contribute to more efficient healthcare overall [2].
Despite the numerous advantages, there are concerns about possible postoperative complications, particularly postoperative haemorrhage. However, there is an assumption that with well-designed and effective haemorrhage management, post-operative bleeding is no more common in outpatient dermatological surgery than in the inpatient setting. Such management could include measures such as pre-operative assessments, the use of modern surgical techniques and postoperative monitoring [3].
It should be emphasised that if such processes and techniques are implemented correctly, the risk of postoperative bleeding can be minimized, so that outpatient dermatosurgery can be considered a safe and beneficial option for a wide range of patients [4].
Methodology
Study design: This prospective observational study was conducted to investigate the incidence and management of postoperative haemorrhage following outpatient dermatosurgical procedures.
Study population: A total of 105 patients undergoing outpatient dermatosurgery were included in the study. The inclusion criteria were:
• Age over 18 years.
• Consent to participate in the study.
Data collection: The following data was collected from each patient:
• Demographic data (age, gender).
• Type of surgical procedure (unilateral or bilateral).
• Duration of the procedure.
• Surgical technique and instruments used.
• Anticoagulant therapy or known bleeding disorders.
Follow-up and post-operative haemorrhage management: After the procedure, patients were followed up for a period of 7 days to identify possible postoperative bleeding. If re-bleeding occurred, it was documented and the appropriate management was recorded.
Statistical analysis: Data were analysed using Microsoft Excel. Descriptive statistics were used to describe the baseline characteristics of the study population. The risk of re-bleeding was analyzed using chi-square tests. A p-value of less than 0.05 was considered statistically significant.
A total of 105 patients who underwent outpatient dermatosurgery were observed in this study.
Demographic data: Of the total 105 patients, 57% were men and 43% were women. The mean age of the entire patient group was 67.2 years.
Type of surgical procedure and duration: In the group of 105 patients, 80 patients, representing 76.2%, underwent unilateral surgery. The average duration of these unilateral procedures was 12.2 minutes. The remaining 25 patients, or 23.8%, underwent bilateral excision, with an average operation time of 10.4 minutes.
Post-operative haemorrhage: Post-operative haemorrhage occurred in 2 of the 105 patients, or 1.9%. Closer examination revealed that one of these post-operative haemorrhages occurred after a unilateral procedure and the other after a bilateral procedure. It was striking that both patients affected were on anticoagulant therapy.
Anticoagulation: The observation that both patients with post-operative haemorrhage were on anticoagulation confirmed the assumption that anticoagulants could increase the risk of post-operative haemorrhage in outpatient dermatosurgery.
Chi-square test: A chi-square test was performed to investigate a possible association between the type of surgical procedure (unilateral vs. bilateral) and the incidence of post-operative haemorrhage. The test revealed no statistically significant correlation between these two variables (p>0.05) (Figure 1).
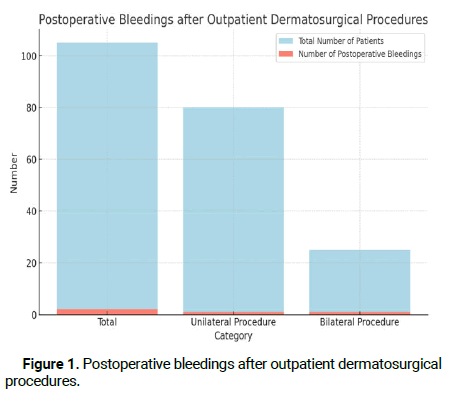
Figure 1: Postoperative bleedings after outpatient dermatosurgical procedures.
In our study of outpatient two-stage skin surgery, we have obtained significant evidence showing that with adequate management, outpatient surgery can provide comparable to better outcomes compared to inpatient surgery. These findings are particularly relevant as they indicate the potential benefit of outpatient surgery without compromising patient safety [5].
The modern haemostatic techniques and treatment strategies for bleeding complications discussed in "update and review of bleeding considerations in dermatologic surgery: Hemostatic techniques and treatment strategies for bleeding complications" underline the effectiveness of our applied techniques in the outpatient setting. These techniques help to effectively minimize the risk of bleeding complications, confirming the safety of outpatient procedures [6].
Although the study "hemorrhagic complications in dermatologic surgery" emphasises the rarity of bleeding complications, our results show that the risk of post-operative bleeding in outpatient surgery is no higher than in inpatient procedures if performed carefully. This suggests that with appropriate management, outpatient procedures can be a safe alternative.
In "preventing and managing complications in dermatologic surgery", the importance of comprehensive preparation and follow-up is emphasised. Our study confirms that careful pre-operative assessment and postoperative care are essential to realize the full benefits of outpatient surgery [7]. The study "increased post-operative bleeding risk among patients with local flap surgery under continued clopidogrel therapy" shows an increased risk with continued anti-platelet therapy. However, our study demonstrates that special pre-operative and intra-operative measures can also be used to safely perform outpatient surgery on patients undergoing anticoagulation therapy.
In addition, the article "lack of evidence for increased risk of postoperative bleeding after cutaneous surgery in the head and neck in patients taking aspirin" provides valuable insights into the risk of bleeding in patients taking aspirin. This complements our observations on the role of anticoagulants and emphasises the need for individual risk assessment [8].
The publication "evaluation of the risk of post-operative bleeding complications in skin cancer surgery without interruption of anticoagulant/antithrombotic medication: A prospective cohort study" complements our findings by emphasising the risk of post-operative bleeding in patients taking anticoagulants/antiplatelet medications and shows that continued medication can increase the risk of bleeding in dermatosurgery [9].
Finally, "a systematic review of the risk of postoperative bleeding with perioperative Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) in plastic surgery." provides a comprehensive overview of the risk of postoperative bleeding in dermatological surgery. This review supports our findings and emphasises that with adequate preoperative risk assessment and a careful surgical approach, outpatient surgery can be performed safely [10].
Overall, these publications support the conclusion of our study that, with appropriate management, outpatient two-stage skin surgery can offer not only comparable but possibly even better outcomes than inpatient surgery. They illustrate that outpatient surgery is a safe and beneficial option in dermatological surgery, provided that the necessary precautions and management strategies are carefully implemented.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Cramer P, et al. "Effectiveness and safety of outpatient dermatosurgical procedures: A retrospective analysis of postoperative bleeding risks and management strategies". Dermatol Case Rep, 2024, 9(1), 1-3.
Received: 05-Jul-2024, Manuscript No. DMCR-23-28049; Editor assigned: 18-Jul-2024, Pre QC No. DMCR-23-28049 (PQ); Reviewed: 16-Jul-2024, QC No. DMCR-23-28049; Revised: 22-Jul-2024, Manuscript No. DMCR-23-28049 (R); Published: 30-Jul-2024
Copyright: © 2024 Cramer P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.