Research Article - (2025) Volume 10, Issue 3
The objective of the study was to evaluate the effect of autologous PRP in the patients of acne scar and its comparison with pretreatment condition on a total of 20 patients. The PRP was prepared in minor OT of Muzaffarnagar medical college and hospital, Muzaffarnagar. The effect of PRP was evaluated by using Goodman's and Baron's qualitative acne scar grading system and compared before and after treatment condition (at 0 and 15 weeks).
Regenerative medicine • Biological interventions • Cellbased therapies • Tissue engineering • Strategy
A two-decade long research has expedited knowledge about tissue repair mechanisms and the field of regenerative medicine is gaining ground stimulated by novel insights and the development of therapeutic biotechnologies, intending to restore tissue architecture and functionality. Regenerative medicine technologies concern not only traumatic tissue injuries but also involve the biological manipulation of pathological conditions aiming to drive tissue circumstances to normal, i.e. the recovery of tissue homeostasis [1]. Biological interventions in regenerative medicine fall into four main categories including gene therapy, tissue engineering, cell-based therapies and Platelet Rich Plasma (PRP) therapies, with different success in clinical translation. In this study we are focussing on PRP therapy in acne scar [2].
Platelet Rich Plasma (PRP) has been used over the last several years as an effective treatment in various surgical and medical fields. The pivotal discovery of Platelet Derived Growth Factor (PDGF) in promoting wound healing, angiogenesis and tissue remodeling threw light on this novel autologous therapeutic modality [3]. Autologous platelet rich plasma has attracted attention in various medical fields recently including orthopaedic, plastic and dental surgeries and dermatology for its various activities, especially in skin rejuvenation, acne scar, alopecia and non-healing ulcer. Dermal stimulation and augmentation represent the main treatments in aesthetic medicine and their use continues to increase [4].
PRP is an effective concentration of multiple fundamental Growth Factors (GFs) by virtue of platelets alone (stored as granules in platelets) and plasma proteins, namely fibrin, fibronectin and vitronectin, that can be produced from whole blood through multiple commercially available systems, resulting in varying levels of platelet concentration. This cocktail of GFs is pivotal in modulation of tissue repair and regeneration, whereas the plasma proteins act as a scaffold for the connective tissue and epithelial migration [5].
The substantial concentration of platelets, compared to normal blood, represents a unique source of growth factors. After its injection into the targeted tissue, such as the dermis and the subcutaneous layers, the platelets are activated endogenously by the coagulation factors normally present in these tissues [6]. This activation leads to a significant degradation of the platelets, which promotes the release of a series of growth factors such as: PGDF, ILGF, EGF and TGFβ. The activated platelets also release numerous proteins, binding to their specific cellular receptors, the glycoproteins and the growth factors activate the intracellular processes that may stimulate cell proliferation, migration, survival, as well as the production of extra-cellular matrix proteins. All these processes contribute to tissue rejuvenation [7]. Platelet rich plasma could act synergistically with growth factors induced by skin needling in order to enhance response. The combination of treatments, carried out by using both skin needling and PRP application enhances its efficacy. So the present study has been planned to assess the effect of autologous PRP in the management of alopecia, acne scar and non healingulcer [8].
In spite of all previous studies regarding use of PRP in different disorders of dermatology, the precise mechanism by which PRP shows its favorable effect has not been properly studied. No studies have attempted to define the specific effects of PRP on skin disorders. The aim of this study was to determine the effects of PRP by using appropriate technique and protocol for real outcome and its comparison with pretreatment conditions [9].
A total number of 20 patients of acne scar of both genders ranging from age 18-60 years were taken under this study, attending OPD at a period of 18 months, in the department of dermatology, venereology and leprology at Muzaffarnagar medical college and hospital. All the patients were explained about the procedure in detail. A consent form was signed by each patient and all the patients were followed by 3 weekly intervals for duration of 15 weeks. All the patients received 5 sessions of PRP after taking approval from institutional ethical committee [10].
Inclusion criteria:
• Patient with realistic expectation
• Patients for aesthetic purpose
Exclusion criteria:
• Critical thrombocytopenia (low platelet count)
• Hypofibrinogenaemia
• Hemodynamic instability (collapse)
• Acute and chronic infections
• Chronic liver disease
• Anti-coagulation therapy (warfarin, dabigatran, heparin)
• Corticosteroid therapy
• Pregnancy immunocompromised state
• Active viral infection at site of procedure and history of keloid scarring
In this study which includes 20 patients, we graded the acne scars of patients by using "Goodman's and Baron's qualitative acne scar grading system" and compared pre and post treatment condition (at 0 and 15 weeks) after injecting 10 ml PRP subcutaneously by pre and post improvement photographs taken with digital camera and also by evaluating Patients Satisfaction Score (PSS), Photograph Score (PS) and Physician Satisfaction Score (PhSS) (Table 1) [11].
| Grades of post-acne scarring | Level of disease | Clinical features |
|---|---|---|
| 1 | Macular | These scars can be erythematous, hyper or hypo pigmented flat marks. They do not represent a problem of contour like other scar grades but of color |
| 2 | Mild | Mild atrophic or hypertrophic scars that may not be obvious at social distances of 50 cm or greater and may be covered adequately be makeup or the normal shadow of shaved beard hair in men or normal body hair if extra facial |
| 3 | Moderate | Moderate atrophic or hypertrophic scars that may not be obvious at social distances of 50 cm or greater and may be covered adequately be makeup or the normal shadow of shaved beard hair in men or normal body hair if extra facial, but is still able to be flattened be manual stretching of the skin |
| 4 | Severe | Severe atrophic or hypertrophic scars that may not be obvious at social distances of 50 cm or greater and may be covered adequately be makeup or the normal shadow of shaved beard hair in men or normal body hair if extra facial and is not able to be flattened be manual stretching of the skin |
Table 1. Goodman's and Baron's qualitative acne scar grading system.
The improvement result obtained and calculated by confronting following parameters patient satisfaction score, physician satisfaction score and photograph score (none=0, mild=2, good=4, very good=6 and excellent=8). Finally Definitive Graduated Score (DGS) (none=0-4, mild=5-8, good=9-16, very good=17-24, excellent=25-36) was found for each patient by adding the final result of each single parameter [12].
Preparation of PRP
PRP and PPP were prepared using a double-spin method and the blood was collected in special sterile vacutainer tubes containing an anticoagulant Na citrate 3.8%, which centrifugally separates red blood cells from plasma that contains ‘buffy coat’ (white blood cells and platelets) [13]. Each test tube was centrifuged at 1100 rpm for 6 min at room temperature. The plasma was gently aspirated from each test tube into a syringe and transferred to a second tube then centrifuged again at 3000 rpm for 10 min at room temperature, thus obtaining a two-part plasma: the upper part, consisting of platelet poor plasma and the lower part, consisting of PRP. The platelet-poor plasma was first gently aspirated to avoid its mixing up with the PRP. The residual PRP was subsequently aspirated from each test tube and prepared for activation by calcium chloride in the proportion of 0.1 ml of CaCl2 per 0.9 ml of PRP, thus obtaining a concentration of activated PRP. Before injection, the target skin surface was cleansed thoroughly with alcohol pads. Topical anaesthetic (tetralid) cream was applied 1 h before injection. Approximately, 3 ml of PRP was produced per tube; this activated PRP was then injected intradermally through a 30 G needle.
When used for filling, the intradermal injections were performed with an insulin syringe.
It is necessary to perform a slight overcorrection of 20%. The amounts injected vary from 4 ml to 6 ml for a face, depending on the patient. Around 1 ml to 2 ml of PRP are injected in two layers over the treatment area. Following injection, Auriderm × 0 (vitamin K) cream or its equivalent, may be applied [14].
In the present study we demonstrated the effect of PRP in 20 patients of acne scar who attended the OPD department of dermatology and VD at Muzaffarnagar medical college and hospital between 1st November 2014, 30th April 2015. The results were statistically analyzed using the paired student t test and ANNOVA. The data was presented as mean ± SD and p value were calculated referring to appropriate tables. The values of p<0.05 were considered as statistically significant [15].
All patients completed the study, including the 3 months follow-up. Most patients had mixed type of acne scars which included: Ice picks, boxcar and rolling scars. The patients were graded into 0-4 grades and estimated the improvement by using Goodman and Baron's qualitative acne scar grading system at all visits (0 week, 3rd week, 9th week, 12th week and 15th week). Out of 20 patients, 10 patients had grade 4 and rest 10 patients had grade 3 before treatment, at the end of the session, all patients showed improvement with grade 1 and 2. The mean ± SD of Goodman and Baron's grading system for acne scar was 3.5 ± 0.512 at 0 week prior to PRP session, whereas after last visit of PRP treatment at 15th week it was 1.55 ± 0.506 which was statistically highly significant (p<0.0001) (Tables 2 and 3).
| Number of patients | Grade | |
|---|---|---|
| 0 Week | 15 Week | |
| 1 | 3 | 2 |
| 2 | 4 | 1 |
| 3 | 4 | 2 |
| 4 | 3 | 1 |
| 5 | 3 | 1 |
| 6 | 4 | 1 |
| 7 | 3 | 1 |
| 8 | 4 | 2 |
| 9 | 4 | 1 |
| 10 | 3 | 2 |
| 11 | 3 | 2 |
| 12 | 3 | 1 |
| 13 | 3 | 2 |
| 14 | 4 | 2 |
| 15 | 3 | 2 |
| 16 | 4 | 1 |
| 17 | 4 | 2 |
| 18 | 4 | 2 |
| 19 | 3 | 2 |
| 20 | 4 | 1 |
| Mean ± SD | 3.5 ± 0.512 | 1.55 ± 0.506 |
| T-test | 11.48 | |
| P value | <0.0001 | |
| Df | 19 | |
| CI | 99% | |
Table 2. Assessment of the effect of PRP on acne scar by using Goodman and Baron's qualitative acne scar grading system.
| Number of patient | Patient satisfaction score | Physician satisfaction score | Photographic score | Definitive graduated score |
|---|---|---|---|---|
| 1 | 4 | 6 | 6 | 16 |
| 2 | 0 | 0 | 0 | 0 |
| 3 | 2 | 2 | 2 | 6 |
| 4 | 4 | 4 | 4 | 12 |
| 5 | 4 | 6 | 6 | 16 |
| 6 | 4 | 4 | 4 | 12 |
| 7 | 4 | 4 | 4 | 12 |
| 8 | 2 | 4 | 4 | 10 |
| 9 | 2 | 2 | 2 | 6 |
| 10 | 4 | 6 | 6 | 16 |
| 11 | 2 | 2 | 2 | 6 |
| 12 | 2 | 2 | 2 | 6 |
| 13 | 6 | 4 | 4 | 14 |
| 14 | 6 | 6 | 6 | 18 |
| 15 | 6 | 6 | 6 | 18 |
| 16 | 0 | 0 | 0 | 0 |
| 17 | 6 | 6 | 6 | 18 |
| 18 | 6 | 6 | 6 | 18 |
| 19 | 0 | 2 | 2 | 4 |
| 20 | 8 | 8 | 8 | 24 |
| Mean ± SD | 3.6 ± 2.30 | 4 ± 2.2 | 4 ± 2.24 | 11.6 ± 0.49 |
| F-test | 77.9 | |||
| Df | 19 | |||
| P value | <0.0001 (highly significant) | |||
| CI | 19% | |||
Table 3. Comparison between PS, PSS, PHSS and DGS improvement scores at 15th week.
The improvement result was also obtained by confronting these 3 parameters: Patient Satisfaction Score (PSS), Physician Satisfaction Score (PhSS) and Photograph Score (PS), which were calculated as follows: 0=none, 2=mild, 4=good, 6=very good, 8=excellent. Finally the Definitive Graduated Score (DGS) was found for each patient by adding the final result of each single parameters. The DGS improvement result was calculated as follows: 0-4=none; 4-8=mild; 8-16=good; 16-24=very good; 24-36=excellent. The result were highly significant (p<0.0001) on 99%confidence interval (Figures 1 and 2).
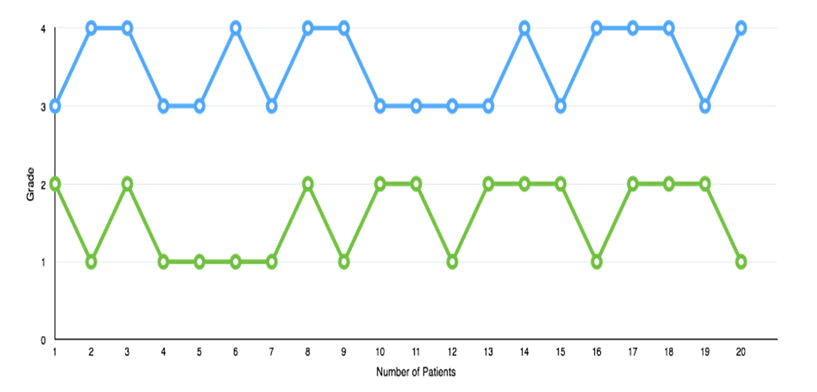
Figure 1: Assessment of the effect of PRP on acne scar by using Goodman and Baron’s qualitative acne scar grading system.
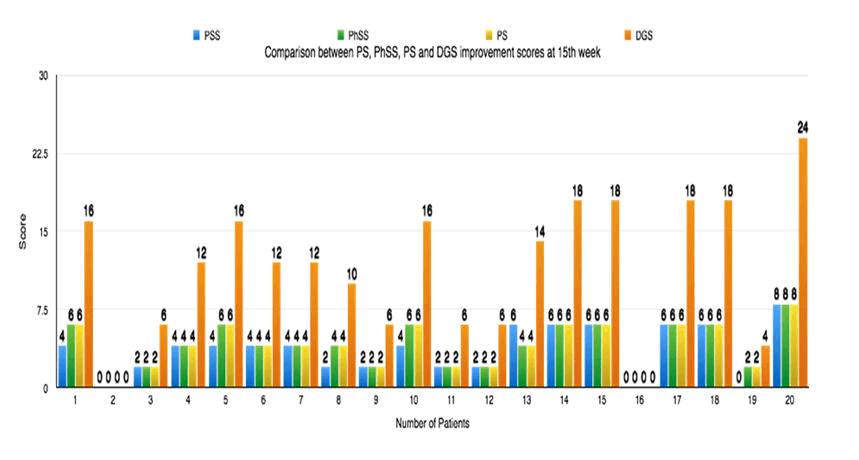
Figure 2: Comparison between PS, PhSS, PS and DGS improvement score at 15th week.
Patient Satisfaction Score (PSS)
A final PSS was calculated on the basis of an anonymous record filled by patient at 15th week and its final improvement average was 3.6. Maximum number of patients (35%) showed good result (score 4) (Table 4).
| Number of patients (n=20) | Percentage of patients (100%) | Result | Score |
|---|---|---|---|
| 3 | 15% | None | 0 |
| 5 | 25% | Mild | 2 |
| 6 | 30% | Good | 4 |
| 5 | 25% | Very good | 6 |
| 1 | 5% | Excellent | 8 |
Table 4. Patient satisfaction score.
Physician Satisfaction Score (PhSS)
The result was obtained considering the photographs evaluation and the patient examination. The degree of satisfaction shown in the final doctor's satisfaction was superior in the degree of satisfaction obtained to the one reported in the PSS. The average result was 4% and 35% patient showed good result (score 4) and 30% patient showed very good result (score 6) (Table 5).
| Number of patients (n=20) | Percentage of patient | Result | Score |
|---|---|---|---|
| 2 | 10% | None | 0 |
| 5 | 20% | Mild | 2 |
| 5 | 35% | Good | 4 |
| 7 | 30% | Very good | 6 |
| 1 | 5% | Excellent | 8 |
Table 5. Physician satisfaction score.
Photograph Score (PS)
After comparing pre and post treatment photographs at 0 and 15th week, the final average improvement of the photographs result was 4%and 65% patient showed effect ranged from good to very good (Figures 3-10 and Table 6).

Figure 3: Acne scar (before).
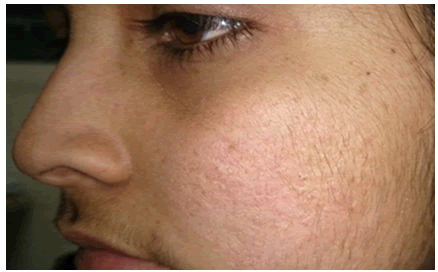
Figure 4: Acne scar (after).

Figure 5: Acne scar (before).

Figure 6: Acne scar (after).
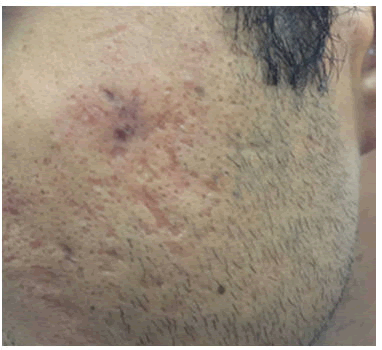
Figure 7: Acne scar (before).

Figure 8: Acne scar (after).

Figure 9: Acne scar (before).
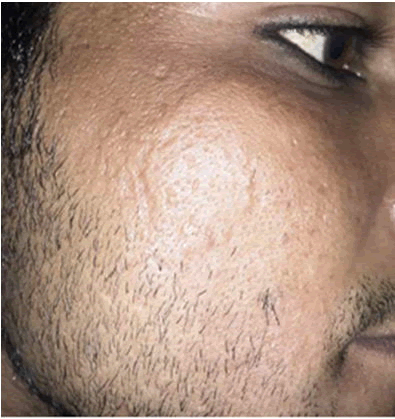
Figure 10: Acne scar (after).
| Number of patients (n=20) | Percentage of patient | Result | Score |
|---|---|---|---|
| 2 | 10% | None | 0 |
| 5 | 20% | Mild | 2 |
| 5 | 35% | Good | 4 |
| 7 | 30% | Very good | 6 |
| 1 | 5% | Excellent | 8 |
Table 6. Photographic score.
Definitive Graduated Score (DGS)
A DGS was calculated by adding PSS, PhSS and PS. The DGS result was good (average 11.6). 40% patient showed good result (score 9-16) and 25% showed very good improvement (score 17-24) (Table 7).
| Number of patients (n=20) | Percentage of patients | Result | Score |
|---|---|---|---|
| 3 | 15% | None | 0-4 |
| 4 | 20% | Mild | 4-8 |
| 8 | 40% | Good | 9-16 |
| 5 | 25% | Very good | 17-24 |
Table 7. Definitive graduated score.
Platelet rich plasma is an autologous product derived from whole blood through the process of gradient density centrifugation. Although the optimal PRP concentration is unclear, the current method by which PRP is prepared involves 300-700 enrichment with platelet concentration consequently increasing to more than 1,000,000 platelet/μl. Autologous PRP has be shown to be safe and effective in promoting the natural process of wound healing, soft tissue reconstruction, bone reconstruction and augmentation. PRP provides an immediate surgical haemostatic agent that is biocompatible, safe and effective. PRP accelerates endothelial, epithelial, epidermal regeneration, stimulates angiogenesis, enhances collagen synthesis, promotes soft tissue healing, decreases dermal scarring and enhances the haemostatic response to injury and decrease the inhibition of wound healing by glucocorticoid. The high leukocyte concentration of PRP has an added anti-microbial effect. The potential value of PRP lies in its ability to incorporate high concentration of platelet growth factors as well as fibrin into graft mixture. PRP has attracted attention in several medical fields in recent years especially dermatology, in conditions like: Striae distensae, lichen sclerosis, lipodermatosclerosis, connective tissue disease associated ulcer, skin rejuvenation, contour defects, acne scars, wound ulcer, alopecia aereata and androgenic alopecia. In present history we only focused on acne scar which are associated with a significant amount of psychological distress both in men and women.
Acne scars are dermal depressions commonly caused by destruction of collagen after inflammatory acne. Many therapeutic measures such as chemical peeling, subcision, dermal abrasions, fillers and punch techniques have been performed to improve acne scarring but with suboptimal outcomes. Ablative lasers such as ER-YAG lasers or CO2 lasers produce significant improvement at the cost of long recovery times and cost effectiveness and post inflammatory hyperpigmentation.
In last few years many studies has claimed roll of PRP in the treatment of acne scar without significant side effects. Gabriella, treated facial acne scar of 12 patients with combined use of skin needling and PRP. It was administered to the participants once at every 8th week for 32 weeks and showed a significant result without any adverse effects. Kim, used intradermal radiofrequency combined with autologous PRP in the treatment of striae distensae once every 4 weeks. The application of PRP not only accelerated recovery and reduce adverse events such as arrythmias and edema, but also enhanced localized collagen neogenesis and redistribution. All participants showed satisfactory changes. Lee, conducted a split face trial which included 14 Korean participants that treated acne scars with PRP ablative CO2 fractional resurfacing and found overall degree of significant improvement. Jiang-Ting, also conducted a study on use of autologous PRP with fractional laser therapy for facial acne scar and demonstrated excellent or marked improvement at the end of treatment.
In present study we graded all the patients into 1-4 grade by using Goodman and Baron's qualitative acne scar grading system before starting treatment at 0 week of which the mean was 3.5 ± 0.512 and estimation of improvement with similar grading system was also done at the end of treatment and the mean was 1.55 ± 0.506 which showed improvement by grade mean 1.95. Final PSS was 3.6, ranging from moderate- good improvement. The final PhSS was 4 ranging from good-very good improvement. The final average improvement of photographs result was also 4 and the DGS was calculated by comparing pre and post improvement photographs, the PSS, PhSS which was 11.6 corresponding to good improvement. This response of PRP in treating acne scar is most likely because of increased proliferation of human dermal fibroblast, increased production of pro-collagen type 1 peptide and expression of collagen type1 which leads to synthesis of new collagen and result in improvement.
In current study PRP was found to be useful in treating acne scar. However, further controlled randomized prospective clinical trials are necessary to definitely demonstrate its efficacy. There is also a need for the development of a standard protocol for the preparation of PRP as literature currently there is no standardization of the procedure. To maintain the result we suggest series of more than 5 sessions with an interval of 3 weeks in between twice a year. Thus, further studies are needed with a longer follow-up and their comparison with standard treatments.
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Mian NZ. "Open Labelled Case Series on the Effect of Platelet Rich Plasma on Acne Scars in Skin of Color ". Dermatol Case Rep, 2023, 8(1), 1-7.
Received: 10-Aug-2020, Manuscript No. DMCR-20-5969; Editor assigned: 14-Aug-2020, Pre QC No. DMCR-20-5969(PQ); Reviewed: 28-Aug-2020, QC No. DMCR-20-5969; Revised: 01-Mar-2023, Manuscript No. DMCR-20-5969(R); Published: 29-Mar-2023
Copyright: © 2023 Mian NZ. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.