Research Article - (2024) Volume 15, Issue 8
Background: The incidence of diabetes is increasing at an alarming rate throughout the world and poses clinical challenges globally; diabetes is recognized as a syndrome characterized by hyperglycaemias and glucose intolerance, and most patients live in low- and middle-income countries. Poor glycaemic control is a major public health issue among patients with type 2 diabetes mellitus and a significant risk factor for the progression of diabetic complications. Glycaemic control and identifying factors associated with diabetes will help health care providers design programs that improve the quality of services provided to diabetic patients.
Objectives: The aim of this study was to assess the magnitude of glycaemic control and its associated factors among type 2 diabetes mellitus patients in Jimma Medical Center.
Methods: An institution-based prospective longitudinal study was conducted on 420 type 2 diabetic patients who were admitted to diabetic clinics at the Jimma Medical Center Clinic from May to October 2023. The data were collected through a structured interview questionnaire and a data abstraction format. The data were entered into Epidata version 4.6 and analysed using SPSS version 26 statistical software. Binary logistic regression was used to explore factors associated with poor glycaemic control. Variables with p values < 0.05 were considered to indicate statistical significance.
Results: A total of 420 type 2 diabetic patients were interviewed and followed for three months. The median age of the participants was 54 years (IQR = 40–60 years). Among the study participants, 52.38% were females. The median duration of living with diabetes since diagnosis was 10 years (IQR: 5–16 years). Approximately 58.1% of the respondents had uncontrolled fasting blood glucose levels. The factors that were significantly associated with poor glycaemic control were female sex (AOR = 2.576, 95% CI [2.80- 11.479]), older age (≥ 60) (AOR = 2.024, 95% CI [1.794-4.646]), duration of diabetes >10 years (AOR = 3.036, 95% CI [2.616-8.306]), T2DM on insulin +OHA drug regimen (AOR=2.08, 95% CI [298-3.918]), obesity (AOR = 2.18, 95% CI [(1.218-4.218]), and DM complications (AOR = 3.193, 95% CI [2.324- 6.05]), which were found to be independent predictors of poor glycaemic control.
Conclusion: The proportion of patients with poor glycaemic control was remarkably high at the JMC. Therefore, more effort should be made to
Glycaemic control; Jimma medical center; Diabetes mellitus; Risk factors; Ethiopia
Diabetes Mellitus (DM) is a serious chronic disease that poses clinical challenges globally and is characterized by hyperglycaemia and glucose intolerance [1], resulting from either when the pancreas does not produce sufficient insulin or when the body cannot effectively use the insulin it produces and leads to significant complications, affecting multiple organ systems and significantly reducing the overall quality. The World Health Organization (WHO) defines diabetes as a “metabolic disorder of multiple aetiology characterized by chronic hyperglycaemias with disturbance of carbohydrate, fat, and protein metabolism resulting from defects in insulin secretion, insulin action, or both”.
Diabetes is a major health issue that has reached alarming levels; currently, more than half a billion people are living with DM worldwide, and diabetes affects individuals across all age groups, races, and socioeconomic backgrounds without discrimination; however, the disease’s impact is notably significant in low- and middle-income countries, where the availability of healthcare, education and resources is constrained. By 2030, 643 million, and by 2045, 783 million adults aged 20–79 years are projected to be living with DM. Type 2 Diabetes Mellitus (T2DM) is the most common type of diabetes, accounting for more than 90% of diabetes cases. Multiple factors contribute to the high prevalence of DM, such as urbanization and physical inactivity, which leads to increased rates of obesity [2].
Good glycaemic control is the cornerstone of diabetes management, as it delays the onset of complications, reduces the cost of care and improves persons with diabetes quality of life. Nevertheless, the control of diabetes remains a challenge worldwide, with only about 50% of the person with diabetes controlled. A recent systematic review of the studies on glycaemic control found: age, sex, poor socio-economic conditions, place of residence, positive family history of diabetes, longer duration of diabetes, treatment modalities and effects, alcohol consumption, smoking, presence of comorbidities or complications, and poor management were associated with poor glycaemic control. Controlling hyperglycaemia is a major therapeutic objective for all DM patients to prevent complications by assessing of the three parameters: glycated haemoglobin (HbA1c), fasting plasma glucose (FPG) and postprandial glucose (PPG) [3].
In recent years, DM has become a problem in developing countries and has contributed to a significant number of deaths in this region. Despite the fact that DM patients benefit from the control of hyperglycaemia, the majority of patients fail to achieve adequate glycaemic control, and the reasons for poor glycaemic control are complex and multifactorial. However, very few studies have been devoted to the factors of glycaemic control in Ethiopia leading to a very rudimentary data on the issue and poor understanding of glycaemic control. In anticipation of the building of an intervention package to deal with the issue in Jimma, and in an effort to expand knowledge about blood glucose control factors, we designed a mixed-method prospective follow up study. Studies with mixed methodology are appropriate to explore complex phenomena in a broad way. Therefore, the aims of this study were to assess the magnitude of glycaemic control and factors contributing to poor glycaemic control among T2DM patients at the JMC [4].
Study area, design and period
An institution-based prospective longitudinal study was conducted among T2DM patients who were admitted to the Diabetic Clinic at Jimma Medical Center (JMC), Ethiopia. JMC is located in Jimma city, Southwest Ethiopia. It is the largest tertiary hospital with specialized services for diabetic patients. It is one of the oldest hospitals and the only teaching and referral hospital in southwest Ethiopia, with a catchment population of more than 15 million people. The hospital has many chronic follow-up clinics for both paediatrics and adult patients. The endocrinology unit in the hospital had two clinic visits every week for patients with T2DM, and the average number of patients attending the clinic in one month was estimated to be 643. The diabetes clinic runs twice weekly (on Monday and Tuesdays) and provides integrated diabetic care for diabetic patients. This study was conducted from May 1 to October 1, 2023 at the diabetic clinic of the hospital.
Population
All T2DM patients who were followed up at the chronic care clinic of the JMC were included in the source population. The study population included randomly selected T2DM patients who attended the chronic care clinic of the JMC during the data collection period and met the inclusion criteria. T2DM patients aged 15 years or older with regular follow-up and who had at least 3 or more measurements of fasting blood sugar (FBS) levels in the past year were included in the study. Participants who were not willing to participate, patients with type 1 diabetes, pregnant women, women with gestational diabetes, newly diagnosed T2DM patients or patients with psychiatric problems were excluded from the study.
Sample size determination
The sample size was calculated using a single population proportion formula by considering p=0.5 (estimated 64.1% T2DM with poor glycaemic control, which was reported from a study conducted at Adama Hospital and d (sampling error) = 5% and using a 95% confidence level); the final sample size was 423. A consecutive sampling technique was used to include participants until the required sample size was obtained.
Data collection procedure
The JMC was selected as the study area. A systematic random sampling technique was used to select the study subjects. Eligible study participants were interviewed face to face using structured data collection tools. In addition, a data abstraction format was used to collect information from participants’ medical records. The tools contain information about the socio-demographic characteristics of the patients, their self-care activities, their clinical, behavioural, and psychological characteristics, and a checklist to review the patients’ medical records. The data were first written in English and then translated to the local languages Amharic and Afan Oromo. Finally, the data were translated back to English by different experts to ensure the validity of the tools.
Data collection tools
Questionnaires on socio-demographic variables were prepared, and study participants were interviewed face to face. Tools to assess patients’ self-care activities: The summary of diabetes self-care activities (SDSCA) scale was used. This scale was developed by Toobert and Glasgow; it has acceptable reliability and validity. It contains 12 questions about diet, exercise, blood sugar, foot care, and medication. Patients were interviewed face to face for each question. Tools to assess the diabetic distress level of the study participants: The diabetic distress score (DDS) was used. This scale was developed by Fisher and his colleague. The Diabetic Distress Scale (DDS17), which is composed of 17 questions, was used to assess diabetic distress among the study participants. Checklist to review the patients’ medical records: After the patients had completed their interviews, their respective medical records were reviewed using a checklist to obtain their last three fasting blood glucose measurements, and the treatment regimen patients were receiving [5].
Data management and quality assurance
To ensure data quality, the reliability of the data extraction forms was checked by performing a pre-test on 5% of the T2DM patients, and training was given to the data collectors. The accuracy and completeness of the data were checked daily after the data collection. For data entry Epidata version 4.6 and for data analysis, SPSS version 26 was used. The fasting blood glucose (FBG) levels of the study participants were categorized as controlled (FBG 70-130 mg/dl) or uncontrolled (FBG<70 mg/dl and >130 mg/dl). Adherence to diabetes self-care was categorized into two categories (adherent and non-adherent) based on their average score, and diabetes distress was categorized into (moderate distress and no distress) categories based on average scores. After categorization was completed, each variable was checked for missing values, and a normality test was performed [6].
Data analysis procedures
Descriptive statistics such as frequency, proportion, mean and standard deviation were employed to describe the sociodemographic, clinical, and behavioural characteristics of the patients. Epidata data version 4.6 was used for data entry, and SPSS version 26 was used for data analysis. We used chi-square tests to determine the associations between categorical variables and blood glucose control. To examine factors affecting poor glycaemic control, we performed a multivariate logistic regression analysis. Variables with p < 0.25 according to univariate logistic regression analysis were entered into a multivariate logistic regression analysis model to identify independent factors that affect glycaemic control. Variables with p < 0.05 were considered statistically significant at the 95% confidence level.
Prior to data collection, ethical approval was obtained from the institutional review board (IRB) of Jimma University, Institute of Health Sciences. An information sheet explaining the aim of the study was prepared and read to all eligible participants. Informed consent was obtained from all study participants. For participants aged younger than 18 years, informed consent was obtained from their parents or legal guardians.
Operational definition
Glycaemic control: For the purpose of this study, we categorized the study participants into two groups based on the American Diabetes Association (ADA) recommendations:
Good glycaemic control: fasting blood glucose of 70–130 mg/dl. Poor glycaemic control was defined as a fasting blood glucose level <70 mg/dl or >130 mg/dl [7].
Fasting blood sugar: Blood glucose was measured from venous blood after 8 hours of overnight fasting or longer.
Diabetes distress: If the study participant’s mean item score for “DDS17” is ≥3, this is considered a level of distress worthy of clinical attention.
Adherence to medication: If the study participant took all his/her anti-diabetic medication in the last seven days.
Adherence to diet: If the study participant had followed the recommended diet for 3 or more days in the last seven days.
Adherence to exercise: If the study participant had followed the recommended level of exercise for 3 or more days in the last seven days.
Sociodemographic characteristics
Of the 423 respondents, 420 were included in the data analysis, for a response rate of 99.29%. Three patients whose data were incomplete were excluded from the data analysis. Of the 420 respondents, 220 (52.38%) and 200 (47.62%) were females and males, respectively. The mean age of the respondents was 54 years (IQR 40–60 years). Overall, 283 (67.38%) respondents were married, and 119 (28.33%) had completed secondary school (Table 1).
| Variables | Categories | Frequency | Percentage |
|---|---|---|---|
| Sex | Male | 200 | 47.62 |
| Female | 220 | 52.38 | |
| Age | <40 | 101 | 24 |
| 40–49 | 78 | 18.57 | |
| 50–59 | 113 | 30.47 | |
| ≥60 | 128 | 26.9 | |
| Educational status | Illiterate | 82 | 19.52 |
| Primary school | 119 | 28.33 | |
| Secondary school | 101 | 24 | |
| Collage and above | 130 | 30.95 | |
| Marital status | Single | 76 | 18.1 |
| Married | 283 | 67.38 | |
| widowed | 39 | 9.28 | |
| Divorced/separated | 22 | 5.23 | |
| Social drug use | Alcohol | 101 | 24.1 |
| Chew Khat | 201 | 47.85 | |
| Smoking | 118 | 28.09 | |
| Occupation | Unemployed | 123 | 29.3 |
| employed | 122 | 29.1 | |
| Merchant | 123 | 29.3 | |
| housewife | 52 | 12.38 | |
| Income | ≤1000 birr | 216 | 51.42 |
| >1000 birr | 204 | 48.57 | |
| Health Insurance | Insured | 244 | 58.1 |
| Uninsured | 176 | 41.9 | |
| Distance to a health facility | Nearby | 167 | 39.8 |
| Distant | 253 | 60.2 |
Table 1: Sociodemographic characteristics of the study participants (type 2 diabetes patients, n = 420) at JMC, Jimma, Ethiopia from May 1 to October 30, 2023.
Self-Care Behaviours of the Study Participants
Of the 420 respondents, 263 (52.61%) were taking adequate physical exercise, 354 (84.28%) were not testing their blood glucose level adequately, and 241 (57.38%) of the respondents were not following their general dietary program correctly. A total of 361 (85.95%) respondents were taking their medication as recommended by their doctors (Table 2).
Variables |
Categories | Frequency | Percentage |
|---|---|---|---|
| Compliance to general diet program the in last seven days | >3 days (adequate) | 179 | 42.61 |
| 0–3 days (in adequate) | 241 | 57.38 | |
| Compliance to foot care program in the last seven days | >3 days (adequate) | 316 | 75.24 |
| 0–3 days (in adequate) | 104 | 24.76 | |
| Physical exercise in the last seven days | >3 days (adequate) | 263 | 52.61 |
| 0–3 days (in adequate) | 157 | 37.38 | |
| Compliance to blood sugar testing in the last seven days | >3 (adequate) | 66 | 15.71 |
| 0–3 (in adequate) | 354 | 84.28 | |
| Compliance medication in the last seven days | 7 days (adequate) | 361 | 85.95 |
| < 7 days (in adequate) | 59 | 14 |
Table 2: Summary of diabetic self-care activities (SDSCAs) of the study participants of JMC, Jimma, Ethiopia from May to October 2023.
Knowledge, behavioural and clinical characteristics of the respondents
For diabetes management, 307 (73.1%) of the respondents did not know their target blood glucose level, and 115 (27.38%) of the respondents had no adequate knowledge about the signs and symptoms of hyperglycaemia and hypoglycaemia. Of the total respondents, 302 (71.9%) had less than three follow-ups in the clinic per year. The median duration of diabetes was 11 (IQR 5–17) years. All 420 (100%) respondents were receiving pharmacological therapy for diabetes. Among those who were on medication for diabetes, 242 (57.61%) respondents were taking Oral Hypoglycaemic Agents (OHAs) alone (Table 3).
Variables |
Categories | Frequency | Percentage |
|---|---|---|---|
| Ever attended diabetic education | Yes | 220 | 52.38 |
| No | 200 | 47.61 | |
| Number of follow up to diabetic clinic per year | ≤3 | 302 | 71.9 |
| >3 | 118 | 28.1 | |
| Number diabetic education Sessions ever attended n = 315 | 1–2 times | 174 | 55.23 |
| ≥3 times | 141 | 44.76 | |
| Knowledge of target blood glucose level | Yes | 113 | 26.9 |
| No | 307 | 73.1 | |
| Knowledge of sign and symptoms of hyper and hypoglycaemia | Yes | 305 | 72.61 |
| No | 115 | 27.38 | |
| Alcohol consumption | Yes | 110 | 26.19 |
| No | 310 | 73.8 | |
| Smoking | Yes | 108 | 25.71 |
| No | 312 | 74.28 | |
| Duration of diabetes | <5 years | 94 | 22.38 |
| 5–10 years | 123 | 29.28 | |
| >10 years | 203 | 48.33 | |
| Drug regimen | OHA | 242 | 57.61 |
| Insulin | 135 | 32.14 | |
| Insulin and OHA | 43 | 10.23 | |
| Body mass Index (kg/m2) | Normal (18.5-24.9) | 79 | 18.8 |
| Overweight (25-29.9) | 112 | 26.67 | |
| Obese (>30) | 230 | 54.76 | |
| Blood pressure (SBP/DBP mm hg) | Optimal (<130/80) | 130 | 30.95 |
| Off optimal (>130/80) | 290 | 69.1 | |
| FBS (mmol/L) | Normal range(4-6.1) | 120 | 28.57 |
| Hyperglycaemic(>6) | 244 | 58.1 | |
| Hypoglycaemias (<4) | 56 | 13.33 | |
| DM complications | Neuropathy | 56 | 13.3 |
| Nephropathy | 113 | 26,9 | |
| Retinopathy | 41 | 9.8 | |
| Hypertension | 110 | 26,2 | |
| Heart failure | 12 | 2.9 | |
| coronary heart disease | 38 | 9,1 | |
| cerebrovascular disease | 33 | 7.9 | |
| peripheral arterial disease | 17 | 4.1 | |
| Number of complications | <5 | 265 | 63.1 |
| ≥5 | 155 | 36.9 |
Table 3: Knowledge, behavioural and clinical characteristics of the respondents at JMC, Jimma, Ethiopia from May to October 2023.
Diabetic Distress
Of the 420 interviewed study participants, 164 (38.8%) had moderate diabetic distress worthy of clinical attention. The mean diabetic distress score was 2.98±1.09. Each subscale of diabetic distress is described below.
Magnitude of glycaemic control among the respondents
The mean fasting blood glucose level from the last three clinic visits was used to determine glycaemic control. In the majority of patients, 244 (58.1%) had an average fasting blood glucose in the range of uncontrolled blood glucose. The mean fasting blood glucose (FBS) of the respondents was 167.63 mg/dl ±51.82 mg/dl. The proportion of patients with poor glycaemic control at a FBS >130 mg/dl and a FBS <70 mg/dl was 47.8 (80%) [95% CI: 75.7%-83.5%]; most 239 (78.6%) had a FBS >130 mg/dl, and only five (1.2%) had a FBS<70 mg/dl (Figure 1).
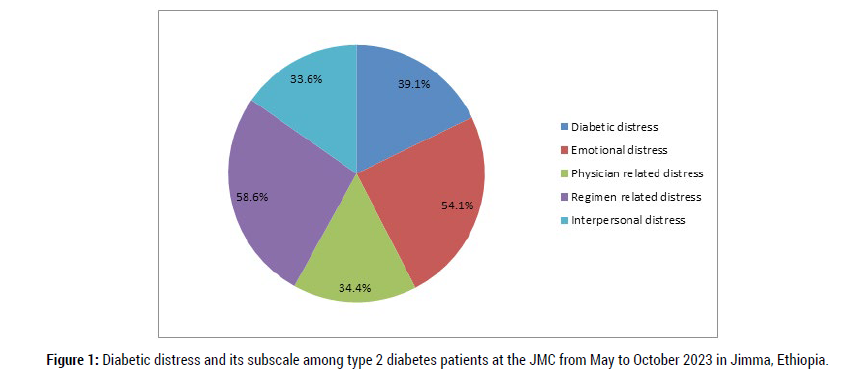
Figure 1: Diabetic distress and its subscale among type 2 diabetes patients at the JMC from May to October 2023 in Jimma, Ethiopia.
Factors associated with poor glycaemic control
Bivariate logistic regression revealed that sex, age, duration of diabetes, drug regimens, body mass index (kg/m2), alcohol consumption, and DM complications were associated with glycaemic control. After controlling of potential confounding factors being female (AOR = 2.576, 95% CI [2.80-11.479], P= 0.001), older age (≥ 60) (AOR = 2.024, 95% CI [1.794-4.646]P=0.002), Alcohols (AOR=2.48, 95% CI [2.391-8.342]P=0.004), duration of diabetes>10 years (AOR = 3.036, 95% CI [2.616-8.306]p=0.003), T2DM on insulin +OHA drug regimen (AOR=2.08, 95% CI [298-3.918],P=0.004), obesity (AOR = 2.18, 95% CI [(1.218-4.218)], P=0.003), having DM complications (AOR = 3.193, 95% CI [2.324-6.05], p=0.002) and poor self-care practices (AOR=3.034, 95% CI [5.821-7.02],P=0.005) were the independent predictors of poor glycaemic control (Table 4).
Variables |
Categories | Glycaemic Control | COR (95%CI) | P value | AOR (95% CI) | P value | |
|---|---|---|---|---|---|---|---|
| Good, n=176 (%) | Poor, n=244, (%) | ||||||
| Sex | Male | 70(39.7) | 177(72.5) | 1 | 1 | ||
| Female | 106(60.3) | 67(27.5) | 3.697(1.088- 1.939) | 0.002 | 2.576(2.08-11.479) | 0.001 | |
| Age | <40 | 22(12.5) | 110(62.5) | 1 | 1 | ||
| 40-49 | 36(20.5) | 73(41.5) | 1.56(.786-3.023) | 0.206 | 0.085(.507-5.613) | 0.29 | |
| 50-59 | 52(29.5) | 91(51.7) | 1.00(.563-4.515) | 0.117 | 1.014(.071-12.186) | 0.8 | |
| ≥60 | 65(36.9) | 93(52.8) | 1.400(.946-10.383) | 0.001 | 2.024(.794-4.646) | 0.002 | |
| Social drug use | Smoking | 46(26.1) | 56(22.9) | 1 | 1 | ||
| Chew Khat | 99(56.3) | 102(41.8) | 2.56(1.786-3.023) | 0.34 | 1.924(2.704-5.626) | 0.23 | |
| Alcohol | 31(17.6) | 86(35.3) | 1.25(.563-4.515) | 0.093 | 2.48(2.391-8.342) | 0.004 | |
| Comorbidity | Yes | 127(72.2) | 100(41.0) | 1.087(1.729-4.406) | 0.86 | 2.229(.794-5.646) | 0.41 |
| No | 49(27.8) | 144(59.0) | 1 | 1 | |||
| Duration of diabetes | <5 years | 49(27.8) | 45(18.4) | 1 | 1 | ||
| 5–10 years | 62(35.2) | 61(25.0) | 1.50(.857-6.373) | 0.096 | 1.005(.627-8.171) | 0.38 | |
| >10 years | 65(36.9) | 138(56.5) | 1.025(.957-5.809) | 0.002 | 3.036(2.616-8.306) | 0.003 | |
| Drug regimen | OHA | 69(39.2) | 82(33.6) | 1 | 1 | ||
| Insulin | 64(36.4) | 79(32.4) | 1.492(.762-2.92) | 0.998 | 1.673(.667-4.197) | 0.189 | |
| Insulin and OHA | 55(31.4) | 83(34.0) | 3.843(.805-4.223) | 0.007 | 2.08(.298-3.918) | 0.004 | |
| Body mass Index (kg/m2) | 18.5-24.9 | 50(28.4) | 44(18.0) | 1 | 1 | ||
| 25-29.9 | 52(29.5) | 75(30.7) | 0.492(1.822-3.82) | 0.22 | 1.623(2.925-5.323) | 0.82 | |
| >30 | 74(42.1) | 125(51.2) | 2.843(1.805-5.223) | 0.024 | 2.18(1.218-4.218) | 0.003 | |
| Comorbidity | Yes | 146(82.9) | 194(79.5) | 0.867(0.934-1.483) | 0.45 | ||
| No | 30(17.1) | 50(20.5) | 1 | ||||
| Number of Comorbidities |
1 | 51(28.9) | 42(17.2) | 1 | |||
| ≥2 | 125(71.1) | 202(82.8) | 1.843(2.215-3.523) | 0.37 | |||
| DM complications | Yes | 138(30.9) | 205(84.1) | 1.023(1.523-4.563) | 0.007 | 3.193(2.324-6.05) | 0.002 |
| No | 28(4.8) | 39(15.9) | 1 | 1 | |||
| Self-care practices | Yes | 97(55.2) | 102(41.8) | 2.843(4.802-6.923) | 0.002 | 3.034(5.821-7.025) | 0.005 |
| No | 79(44.8) | 142(58.2) | 1 | 1 | |||
Table 4: Factors Associated with Poor glycaemic Control in T2DM at JMC from May to October 2023 in Jimma, Ethiopia.
Poor glycaemic control has been associated with a negative impact on diabetic patients and the healthcare system, including increased healthcare costs, increased medication costs, and increased rates of hospitalization. In this study, the mean age of the T2DM patients was approximately 54 years, with the majority of them aged 40–60 years. This age group had a greater proportion of patients with poor glycaemic control than did the <40 years age group. This finding was in line with a study conducted in Tanzania that reported that the mean age of patients with T2DM was 55 years [8]. Other studies have shown that young age is associated with poor glycaemic control. The observed variation in the association between age and poor glycaemic control could be explained by differences in population characteristics and age distributions among different studies.
Overall, the study revealed that glycaemic control among the study subjects was far below the recommended standards. The mean fasting blood glucose level of the study subjects was 167.63 mg/dl ±51.82 mg/dl. This finding is comparable to that of a study conducted in Tanzania 166.9 ± 60.8 mg/dL and Addis Ababa 165.63 mg/dl ±51.82 mg/dl. Evidently, our finding is much greater than the American Diabetic Association recommendation. This study revealed that a high proportion 58.1% of the T had poor glycaemic control. This finding is less than a study conducted in Tanzania (66.1%), Saudi Arabia (74.9%), Mizan-Tepi (64.1%), Sudan 80%, Congo 67.8 and India (91.8%). The proportion of patients with poor glycaemic control in the present study was greater than studies conducted in Haramya 45.2% [9]. The possible explanation for this difference could be that the patients seeking advanced management were referred to Jimma Medical Centre. It is the only hospital in the Southwest Ethiopia where patients were coming from.
In this study, females were 2.576 times more likely to have poor glycaemic control than males were (AOR = 2.576, 95% CI [2.80-11.479], P= 0.001). This finding is in agreement with studies conducted in Kenya [10], which implies that fewer women achieved their glycaemic target than men did. The possible explanations might be related to the greater natural deposition of fat in females, which facilitates insulin resistance, than in males, the lower physical activity level of females and the feeding practices of women, in which females usually consume sweet foods with a high glycaemic index in Ethiopia. Additionally, the high calorie food consumed during the puerperal period by females and physiological differences could be sources of gender disparity.
In this study, the odds of poor glycaemic control among T2DM patients who consumed alcohol were 2.48 times greater (AOR=2.48, 95% CI [2.391-8.342], P=0.004) than those among patients who were nonalcoholic. Other studies conducted in Tanzania, Uganda, Bosnia and Herzegovina have also reported a positive association between poor glycaemic control and alcohol intake among diabetic patients. Alcohol intake is detrimental, particularly for vulnerable people such as those with diabetes, and usually affects the ability of patients to practice self-care for themselves as well as vital body organs. Studies have shown that excess alcohol intake, particularly in patients with DM, can lead to the accumulation of certain acids, including acetic acid and acetaldehyde, in the blood circulation, which can lead to lethal complications, including damage to organs, dehydration, and increased blood pressure [11]. Additionally, alcohol intake can worsen diabetes-related medical complications, such as disturbances in fat metabolism, nerve damage, and eye disease.
In this study, overweight T2DM patients were 2.18 times (AOR = 2.18, 95% CI [(1.218-4.218)], P=0.003) more likely to have poor glycaemic control than patients with a normal BMI. The present research agrees with previous findings in South Africa, India, and Ethiopia, possibly because these patients often have higher dietary intakes of food high in carbohydrates and a high glycaemic index, thus enhancing their fat storage and making their glycaemic levels harder to control [12]. This can probably be explained by the fact that obese patients were more likely to have poor glycaemic control than normal BMI patients due to the fact that increased fat mass and visceral adiposity, which affect insulin sensitivity and cause insulin resistance. However, increasing weight could also arise in persons with diabetes due to the effect of antidiabetic medication on body weight. Apart from metformin and thiazolidinediones, other antidiabetic agents could lead to weight gain.
A high proportion of patients with poor glycaemic control were treated with a combination of OHA and insulin (AOR=2.08, 95% CI [298-3.918], P=0.004). This finding is consistent with studies conducted in Ghana, Haramya and Malaysia. Patients with poor glycaemic control require more aggressive treatment with insulin or a combination of OHA and insulin. Patients who are using OHA alone have good glycaemic control compared with those treated with insulin alone or in combination with OHA.
The duration of DM since diagnosis influenced glycaemic control among T2DM patients in our current study. Our study revealed that T2DM patients with duration of DM >10 years have poorer glycaemic control than patients with relatively shorter (< 5 years) duration of diabetes (AOR = 2.72 95% CI: 1.16–6.32). This finding was similar to studies conducted in Malaysia and Iraq. The positive correlation between a longer duration of diabetes and the risk of poor glycaemic control was possibly due to the progressive impairment of insulin secretion with time because of the failure of β-cells, increased insulin resistance to control blood sugar, and eventually decreased insulin secretion, which also impair the body’s response to diet control or oral medication [13], adherence of patients with a shorter duration of the disease to medication and diet.
A greater proportion of patients with poor glycaemic control were in the group of DM with complication (AOR=3.193, 95% CI [2.324-6.05], P=0.002) than in the group of T2DM with without complications. This finding is consistent with studies conducted in the USA, Ghana and Malaysia. The presence of comorbidities/complications poses a problem with respect to pill burden, adherence to treatment and cost, or as an intricate mechanism linked to beta-cell impairment or aggravated insulin resistance. There is a need to focus on managing diabetes-related complications to ensure that those conditions are managed well alongside the diabetes itself to achieve optimal glycaemic control [14].
Moreover, this study also showed that poor self-care activities were 3.034 times (AOR=3.034, 95% CI [5.821-7.02], P=0.005) more likely to be associated with poor glycaemic control than good self-care activities, which was similar to the findings of a study performed in western Ethiopia. This finding is consistent with earlier findings in Kenya, Ethiopia, Jordan and the United States of America [15], which showed that patients who had high self-efficacy were two times more likely to have controlled blood glucose than were those with low self-efficacy. This similarity justifies the fact that effective self-care activities could help individuals attain optimal glycaemic control.
This study revealed a significantly high prevalence of poor glycaemic control among patients with T2DM. Older age, duration of diabetes, drug regimens, body mass index (kg/m2), alcohol consumption, and diabetes mellitus (DM) complications were significantly associated with poor glycaemic control. Special attention should be given to patients with a longer duration of diabetes and those who are receiving insulin therapy.
AOR: Adjusted Odds Ratio; BMI: Body Mass Index; CI: Confidence Interval; COR: Crude Odds Ratio; DM: Diabetes Mellitus; FBS: Fasting Blood Sugar; HbA1c: Haemoglobin A1c; JMC: Jimma Medical Center; SPSS: Statistical Package for the Social Sciences; SD: Standard Deviation; USD: United States Dollar
We would like to thank Jimma University, the data collectors and all the study participants.
None of the authors have competing interests with the material presented in this manuscript.
This research was funded by the Jimma University Institute of Health. The funding body had no role in the design of the study; the data collection, analysis, or interpretation of the data; or the writing of the manuscript.
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Readers who will require the data and materials of the current study can communicate and obtain the data from the corresponding author upon reasonable request.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Received: 19-Jul-2024, Manuscript No. jdm-24-33031; Editor assigned: 22-Jul-2024, Pre QC No. jdm-24-33031(PQ); Reviewed: 05-Aug-2024, QC No. jdm-24-33031; Revised: 09-Aug-2024, Manuscript No. jdm-24-33031(R); Published: 16-Aug-2024, DOI: 10.35248/2155-6156.10001148
Copyright: © 2024 Garedow AW, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.